http://www.ulzibat.ru/en/method/
First of all I want to say that my child did not had this operation ( he don’t have fibrous modified muscle fibers at least not yet 3 years after anoxic injury…. we saw doctor for consultation this summer….but doctor Repetunov said he didn’t need it (at least for the moment).
microfibrilotomy or Ulzibat methode :
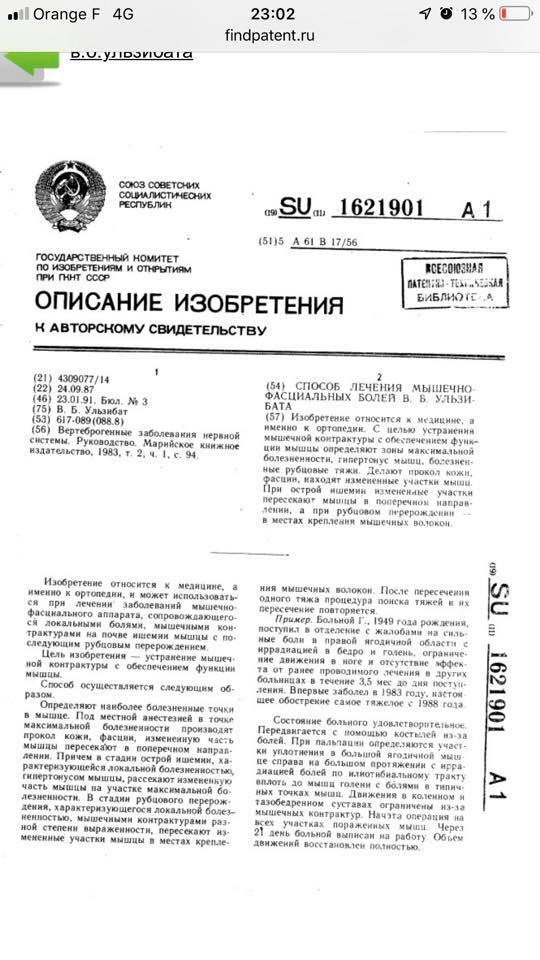
The development and implementation of the method began in 1985 and ended with the drawing up in 1987 of five applications for inventions, which were subsequently registered as patents NoNo 1560143, 1621901, 1641300, 1718868 and 2014020.
This technology is designed to eliminate organic muscle contractures and myofascial pain syndrome. It is based on a phased subcutaneous intersection of fibrous modified muscle fibers in the zone of their attachment to the bone using a special scalpel (microfibrilotomy VB Ulzibata) in order to improve muscle function.
Source :
http://www.oocities.org/ulzibat/russian/novayakniga.htm
Partial translation :
Dr Ulzibat put forward the hypothesis that the sclerotic changes in the myofibrils of the muscle fiber (myofibrillosis) are the basis of the IFB [28]. The pathogenesis of pain syndrome in IFA is formulated taking into account clinical and morphological signs, and is represented by four main mechanisms [29]. The main stages of pathogenesis are as follows: when muscle pathogenic factors of various nature (physical, chemical, biological) are exposed to muscle contraction occurs (MC). SMPB is clinically manifested by weakness, stiffness, increased muscle fatigue. In the future, the continuation of the effect of the damaging factor in the area of localization of MK develop dystrophic and necrotic changes in the myofibrils at the level of the cell, fiber or bundle of fibers, accompanied by the appearance or enhancement of IFB. Then necrotic myofibrils are lysed, and the process of replacing them with parts of the connective tissue inside the remaining cell wall begins. Perhaps the progression of the disease with the involvement of new myofibrils, contractures occur in other areas of the same and other muscles.
The development of the cicatricial process in the thickness of the muscle causes extravascular compression of the blood vessels, leading initially to chronic disturbance of the organ circulation, or during the development of tension – to an acute infarction of a significant part of the muscle tissue, which aggravates the course of the disease and provokes pain. When a nerve is compressed in the thickness of the affected muscle, the pain syndrome increases.
Thus, there are many unresolved and controversial issues in the study of the etiopathogenesis of SMFPs. The pediatric aspect of this problem is particularly important to consider, since it can be key in developing a set of preventive measures, early diagnosis of the initial manifestations of the disease and timely and adequate etiotropic and pathogenetic therapy aimed at preventing the process from becoming chronic, reducing the frequency and severity of manifestations of the disease in adults.
« Dr Ulzibat repeatedly expressed his opinion that the leading cause in the occurrence of chronic and acute pain syndrome is the local dystrophic process of connective tissue, leading to necrosis and the development of scar tissue at the site of necrosis. Therefore, the effectiveness of a particular method of relieving pain depends mainly on what stage of the pathological process it started: in the initial stage – the « loose » scar (functional, muscular-tonic, algic) – any of the above methods may result to the weakening and disappearance of the pain syndrome due to the improvement of the microcirculation of the affected muscle area, and with continued scarring (aging), conservative methods are not very promising [6].
This cicatricial process in skeletal muscles leads to the development of a variety of fibrous contractures, hidden and obvious.
They stimulate the development of movement disorders and the formation of antalgic postures in the patient. The more cicatricial changes and, consequently, the rougher the contracture, the more pronounced the pain syndrome. »
Part 2:
In this part : they did analysis of method in one small Russian city (only 59 patients in 2 day operation )
АНАЛИЗ ЭФФЕКТИВНОСТИ ПОЭТАПНОЙ ФИБРОТОМИИ В ЛЕЧЕНИИ ДЕТЕЙ С СИНДРОМОМ МЫШЕЧНО-ФАСЦИАЛЬНЫХ БОЛЕЙ (по г.НАБЕРЕЖНЫЕ ЧЕЛНЫ).
Цой Е.В., Бударин В.И., Репетунов А.А., Ульзибат Б.В.
ANALYSIS OF EFFICIENCY METHOD – GRADUAL FIBROTOMY IN TREATMENT OF THE CHILDREN WITH THE MYOFASCIAL PAIN SYNDROME (NABEREZHNIE CHELNI).
In his work we throuhgoutly analysis the contingent of patients which came for treatment to ZAO “Institute of Clinical Rehabilitology” on preoperational and other stages of operative treatment by the method used in our institute- gradual fibrotomy. As an object of the research we chose a group of children from one region- the Naberezhnie Chelni (Tatarstan republic).
We proved that the method – gradual fibrotomy is a method of choice for this category of patients, used in ambulatory-outpatient conditions.
In order to objectify the level of effectiveness of the medical methods of the Institute of Clinical Rehabilitation, it was decided to characterize in detail the contingent of patients who applied for the preoperative and subsequent stages of surgical treatment. A group of children suffering from « cerebral palsy » from one region, the city of Naberezhnye Chelny, was selected as the object of study. This made it possible to avoid difficulties in processing information about patients due to the presence of a unified methodological approach to a patient with cerebral palsy within the same territory.
All children who applied for specialized orthopedic care were examined by a full-time orthopedic surgeon and a children’s neurologist at the institute, and extracts from the children’s development histories provided by the neurologists and orthopedic surgeons of Naberezhnye Chelny were analyzed; interviews were held with parents in order to clarify details of the history of life and illness, which are not reflected in the extracts; timeliness, volume, continuity, efficiency of treatment received by each child in the system of rehabilitation of patients with cerebral palsy were evaluated [13].
33 boys and 26 girls applied to the institute, 57 of them – for the first time, 2 – again.
33 boys and 26 girls applied to the institute, 57 of them – for the first time, 2 – again.
The age distribution is as follows: 1 – 3 years – 4; 4 – 7 years – 30; 8-10 years old – 14;
11-15 years old – 8; over 15 years old – 3.
At the time of inspection, the clinical signs of tetraparesis were observed in 30 people, hemiparesis – in 7 children, lower spastic paraparesis – in 8 children, the hyperkinetic form was diagnosed in 12 patients, the atonic-astatic form – in 2 children.
These data are presented in table №1.
Table number 1. Distribution of children with cerebral palsy by degrees
movement disorders:
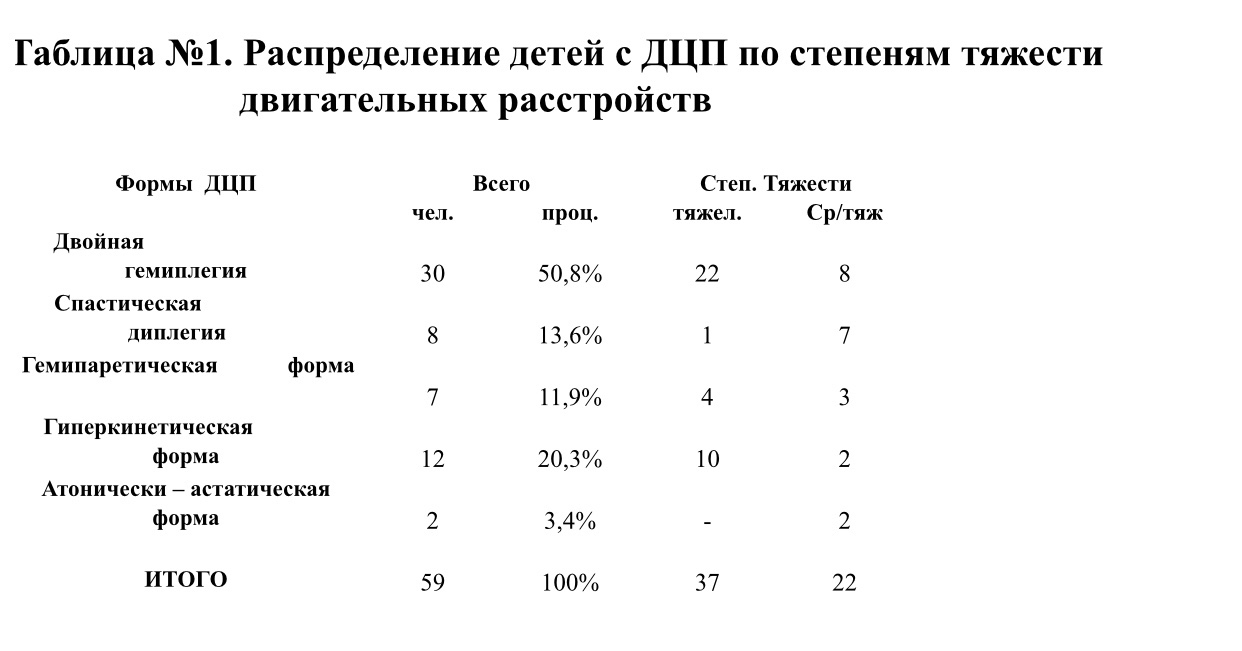
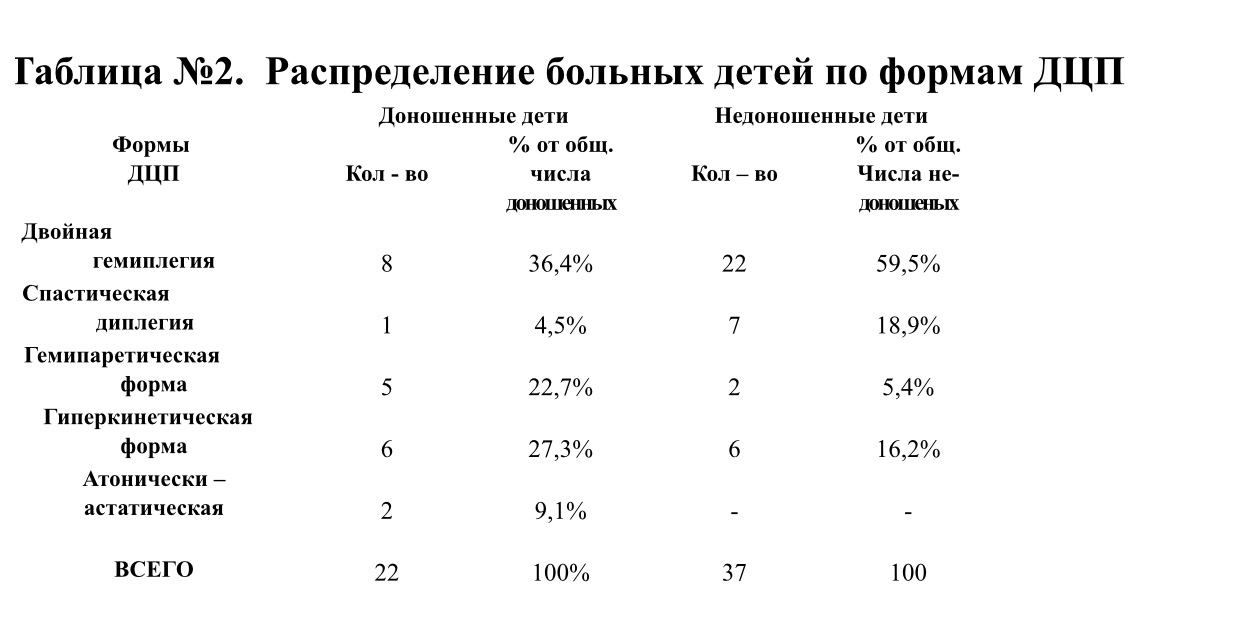
Severe motor impairment was found in 37 (62.7%) children, moderate severity – in 22 (37.3%) children, patients with mild lesions were not. In the subgroup of premature babies, the lesions of a severe degree are determined 2 times more often than moderate ones, in the group of full-term babies the ratio is 1: 1. In 88% of cases there was a bilateral lesion of the muscles of the limbs, torso, face (see table number 2).
Examination of all children in all motor segments and in all muscle groups revealed local zones of consolidation, and palpation of these areas with the most pronounced induration was accompanied by pain. We found the greatest pain in the muscles of the face (temporal and chewing), shoulder girdle, waist and feet [12], [21].
We regard these seals as a manifestation of overt and hidden cicatricial contractures located deep in the skeletal muscles [22].
In addition to the obvious signs of motor impairment, the conclusions of leading experts of Tatarstan in 24 children noted a delay in the intellectual development of varying degrees.
Due to the short duration of the stay of children in the hospital for one day, we did not conduct an in-depth study of higher mental functions. But, based on the organic relationship and interdependence of emotional and cognitive processes as the most important areas of the psyche of children [1], [2], [4], [7], [8], [10], [14], [24], [27], and considering emotions as a psychosomatic phenomenon [7], [8] we decided to pay more attention to assessing the state of the emotional sphere. At the same time, we proceeded from the concept that with difficult speech contact, the analysis of the emotional profile can serve as an objective indicator of the child’s mental development [4], [7], [8], [10], [24], [27]. When assessing emotional and behavioral reactions, we took into account the characteristics of age psychology, psychological characteristics of sick children, the main characteristics of temperament as a set of innate properties of the individual psyche: the prevailing mood background, the level of adaptability and accessibility, the threshold level, the intensity and stability of these reactions, the level of activity. The microsocial background, previous life experience of each child (including the experience of treatment) and the presence of the syndrome of chronic myofascial pain, causing depressive states [5], [6] were also taken into account.
The emotions shown by the patients of this contingent during the contact (speech, gestures, mimic, mixed) covered the maximum possible spectrum, were individually-evaluative in nature and were quite complex, differentiated. The reaction of the children to the new environment, new people, the situation, orthopedic and neurological examination, local pain during palpation of the muscles was adequate.
Delayed speech development was observed in 24 children, alalia – in 3 children, dysarthria – in 14. Many children had the so-called combined syndromes [1], [2], [14], [17]: convulsive – 21 children, hydrocephalic – 6 children, visual impairment in the form of refractive errors – 33 people, Å, squint – 30, 11 children had a lack of weight and height.
According to the available information obtained in an interview with parents and confirmed by data from outpatient developmental cards of children, 22 mothers of children with cerebral palsy had a burdened obstetric history (preterm birth, miscarriage, abortion, infertility). Five mothers and nine fathers had occupational hazards at the time of conception, one mother and five fathers suffered from chronic diseases. In three children, heredity of cerebral palsy was burdened by the father and mother. 23 children were born from the first birth, 36 – from repeated. In 43 cases our patients have healthy brothers and (or) sisters, in 33 cases they are older than a sick child, in 10 cases they are younger. In 16 families, the sick child is the only one.
In the history of 7 mothers, there were indications of the threat of termination of this pregnancy, acute infectious diseases – in 9 in the first half of pregnancy, in 6 – in the second half of pregnancy, early toxicosis – in 8, toxicosis of the second half (dropsy, nephropathy) – in 7 , anemia – in 11. Ten women during pregnancy was prosperous.
Premature birth occurred in 37 cases (62.7%), 18 (30.5%) children were born full-term, 4 (6.8%) were post-mortem, 5 (8.5%) children had a mass deficit in terms of gestation. Twenty children were born in gestational age of 26-31 weeks, 12 children were born in the period of 32-34 weeks, 5 – in the period of 35-37 weeks (classification of the degree of prematurity by gestational age) [25].
Table number 3. Distribution of children with cerebral palsy by severity
motor disorders depending on the period
gestation

T – severe, C – moderate.
57 women had independent births (of which 6 were swift), and 2 women were operational. 50 children were born in headache presentation, 7 – in the buttock, 2 – in the sheath & ## 1086; m. There were five children from multiple pregnancies (three of the dizygotic twins, two of the monozygous twins). Of the three dizygotic twin pairs, three children are our patients (one of them has a hyperkinetic form of moderate severity, the second has a moderately severe tetraparesis, and the third has a lower spastic paraparesis of moderate severity); of the remaining three children, one is healthy, one died antenatally, one died on the first day of life. Two boys from monozygous twins are sick: the first one shows signs of severe tetraparesis, the second one has lower spastic paraparesis.
Nine women were given birthstimulation due to the weakness of labor, five indicate the fact of squeezing of the fetus, seven had a long, dry period. 57 (96.6%) children had signs of asphyxia at birth [26]. Seven were given artificial lung ventilation (4 of them show signs of severe tetraparesis and 1 – hemiparesis of moderate severity, in 2 – a hyperkinetic form of severe and moderate degree). In 3 children, the cord was entwined around the neck, and in 2 children, cephalhematoma was detected. Two children after birth received treatment for hemolytic disease of the newborn, incompatibility according to the Rh factor (in 1 – severe tetraparesis, in 1 – hyperkinetic form of moderate severity). At discharge from the neonatal pathology department, 18 children were diagnosed with intrauterine or atelectatic pneumonia, 28 were diagnosed with CNS birth trauma, 6 children had a combination of these diagnoses.
Cerebral palsy was diagnosed in the first year of life for 25 children (10 in the first half of the year, 15 in the second); in the second year of life – 23, in the third – 6, in the fourth – 5.
Conservative therapy, including drug treatment, massage, therapeutic gymnastics, physiotherapy, reflexology, gypsum and other methods [19], started before 1 year 39 (66.1%) for children (up to 6 months – 29, from 6 to 12 months – 10), from 1 year to 2 years – 17 (28.8%), from 2 to 3 years – three (5.1%). Of the 39 children who underwent complex conservative therapy in the first year of life, 26 children (two thirds), however, at the time of admission to the institute, have signs of severe motor impairment: in 15 – by the type of tetraparesis, in 3 – hemiparesis, in 1 – lower spastic paraparesis, in 7 children – hyperkinetic form. The moderate degree of damage in 13 children: by the type of tetraparesis – in 5, hemiparesis – in 2, lower spastic paraparesis – in 2, hyperkinetic form – 2, atonic – astatic form in 2.
Of the 17 children who received treatment in the second year of life, 9 had severe motor disturbances (6 had tetraparesis, 3 had a hyperkinetic form), 8 had moderate ones (3 had tetraparesis, 4 had lower spastic paraparesis, 1 had – hemiparesis). Of the three who started treatment at 3, in 1 – severe tetraparesis, in 2 – moderate lower spastic paraparesis. From birth, 15 (25.4%) children are continuously treated, of which 10 (two-thirds) at the time of the examination have a severe degree of lesion, and 5 have a moderate degree.
Comprehensive conservative treatment all children received at an early age almost continuously, at a higher age courses, at least 1 time in 3-6 months.
It is interesting that in four of the 11 children with a history of episyndrome, his debut is associated with receiving injections of cerebrolysin, in 1 child the first convulsive seizure developed at the time of electrophoresis. In 1 boy with severe tetraparesis, convulsions were provoked by massage and therapeutic exercises. In patients with hyperkinetic form, stimulating development of the central nervous system, pharmacotherapy, electric, mud, balneal, and reflexotherapy lead to an increase in hyperkinesis during the treatment period, according to the parents of our patients.
All enrolled children had the desire to move, but out of 59 children, only 20 walk independently with moderate lesions and hemiparesis, and in all cases the gait is defective due to persistent contractures and deformities, 10 children have support and 9 children move on their knees, 8 children crawl on all fours, six children with the commenced and actively pursued complex therapy have mastered only crawling on the stomach, six do not move at all.
All children have multiple overt and covert muscle contractures resulting in fixed contractures of the joints: shoulder, elbow, wrist, metacarpophalangeal, hip, knee, ankle; deformations of feet.
Here’s how parents themselves evaluate the effectiveness of conservative treatment of their children: parents of 16 children expose the “no effect” assessment, parents of 43 children consider ineffective the conservative therapy.
Parents of 12 of 59 children completely abandoned conservative therapy due to its low effectiveness in correcting the existing severe deformities of the joints. Other parents, refusing pharmacotherapy and physiotherapy, resorted to the services of manual therapists, massage therapists, reflex therapists, homeopaths, who promised to consolidate the motor stereotype that was formed.
2 boys reapplied. Kostya S. for 4.5 years, (case history No. 3070), with signs of lower spastic paraparesis of moderate severity – for the 4th stage of surgical treatment.
Kostya S. first entered the institute in May 1994 at the age of 1 year and 9 months, when the boy himself sat uncertainly, did not stand up, did not stand, was disturbed by a pronounced crossing of the lower extremities, relying on the front sections of the feet, the absence of phrasal speech and pronounced drooling. The therapy carried out since birth (medical, therapeutic exercises, massage, physiotherapy, acupuncture, the use of the Adele medical suit) gave a temporary effect. After stage 1 of the operative treatment, the boy began to sit well, the range of movements in the hip and ankle joints increased, phrasal speech appeared, drooling disappeared after micro-operations on the chewing and temporal muscles. After stage 2 (September 1994) the boy began to get up on his own, walk at the support and with support for 2 two hands, after stage 3 (December 1995) – walks with support for 1 arm and takes the first independent steps.
Daniel B., 8 years old (case history No. 6654) entered the 2nd stage of treatment. Diagnosis: cerebral palsy. Double hemiplegia, severe. Delayed intellectual development. Alalia Episindrom. Hypotrophy. This patient of our patient had much more in accordance with the clinical diagnosis at admission, and the goal of surgical treatment, pursued by parents-doctors when applying to the institute, was more modest than in the 1st case: relief of patient care and reduction of pain . Combined therapy (massage, gymnastics, pharmacotherapy, acupuncture, laser puncture, microwave resonance therapy, homeopathic remedies), carried out systematically since 4 months, had no effect. The main complaints on admission to the 1st stage of treatment (August 1996): severe anxiety, deep delay in motor and intellectual development, lack of active speech, significant limitation of passive and active movements in all joints of the upper and lower extremities, impaired hand manipulative function (lack finger grip), a violation of chewing, swallowing, salivation, poor sleep, restless sleep. After the 1st stage, the boy became calmer, sleep returned to normal, the range of movements in the shoulder, hip, knee joints increased, the manipulative function of the hand improved (finger grasp appeared), the mobility of the tongue increased, the chewing, swallowing, and salivation decreased.
In June, the 2nd stage of treatment was received on the recommendation of doctors from Naberezhnye Chelny, who observed our patients in the early postoperative period, 7 children from those operated on in January-February 1997: 5 with severe tetraparesis, 2 with severe and moderate hyperkynetic form degree. The results of the 1st stage are positive: 5 of 7 children have a transition to a new level of motor development [17]. All children increased the volume of movements in the operated limb segments.
Here is a reflection of the dynamics of symptoms after the 1st stage of treatment according to the method of V. B. Ulzibat in each of 7 children [20].
Elvira M., 7 years old (case history No. 7039). Diagnosis: cerebral palsy. Double hemiplegia, severe. Hyperkinetic syndrome. Dysarthria. Effects of the 1st stage: reduction of shoulder, hip, ankle joint contractures, improvement of speech.
Andrei O., 7 years old (case history No. 7042). Diagnosis: cerebral palsy. Double hemiplegia, severe. Delayed intellectual and speech development. Pseudobulbar syndrome. Episindrom. Effects: reduction of shoulder, hip, knee, ankle joint contractures; the boy learned to stand up without support, began to crawl confidently on his knees, the manipulative function of the brush, posture improved, interest in games appeared; speech and chewing – without dynamics.
Anatoly R., 11 years old (case history No. 7043). Diagnosis: cerebral palsy. Double hemiplegia, severe. Hyperkinetic syndrome. Dysarthria. Effects: reduction of shoulder, elbow, hip, knee, ankle joint contractures; He began to sit himself, began to change his posture during wakefulness and in a dream, without help, his speech became more intelligible, his chewing and handwriting improved.
Vyacheslav I., 11 years old (case history No. 7045). Diagnosis: cerebral palsy. Double hemiplegia, severe. Effects: contractures of the shoulders, elbows, hip, knee joints have decreased, they began to stand without support, take the first independent steps, their mood improved, the feeling of fear disappeared.
Roman Sh., 7 years old (case history No. 7041). Diagnosis: cerebral palsy. Double hemiplegia, severe. Dysarthria. Effects: contractures of the shoulder, elbow, hip, knee joints have decreased, began to crawl on all fours, began to sit without support, active movements appeared in the right hand, decreased fear of falling, loneliness, improved speech, chewing, decreased strabismus and severity of foot clones.
Volodya F., 10 years old (case history No. 7173). Diagnosis: cerebral palsy. Hyperkinetic form, moderate. Dysarthria. Effects: decreased severity of torticollis, improved speech, decreased amplitude and severity of nystagmus.
Gulya S., 5 years old (case history No. 7331). Diagnosis: cerebral palsy. Double hemiplegia, severe. Episindrom. Effects: contractions of the elbow, hip, knee, ankle joints have decreased, the girl began to sit herself, the manipulative function of the hands has improved.
CONCLUSION:
According to our data, in most cases, conservative therapy conducted for children from Tatarstan complied with the principles of early onset, phasing, continuity, continuity, complexity and completeness of the volume of rehabilitation measures [3], [13], [14], [19].
In all patients of this group, we identified the syndrome of musculo-fascial pain in the standard points [23], corresponding to the localization of scars in the muscles [12]. At these points, all children showed combined polysegmental fixed contractures, both explicit and implicit, causing the development of motor disorders of varying severity [21].
These movement disorders are not hereditary [19]. With the manifestation of cerebral palsy in monozygous and dizygotic twins, one can recognize the presence of a genetic predisposition to the development of intrauterine pathology [9], [11].
The pathological systemic process that began in the antenatal period in most patients and led to the development of severe movement disorders is one of the causes of miscarriage and premature birth, being a variant of the immunological incompatibility of the mother and fetus tissues [25]. The predominance of severe forms of motor impairment in premature babies is also explained by the peculiarities of their microvasculature functioning in ontogenesis with the development of primary functional heart failure [15], [28], hypovolemia of the large circulation, hypoperfusion of organs and tissues, including skeletal muscles.
The pathology of the antenatal period revealed in a large percentage of cases (83% of cases showed a complicated course of pregnancy) ultimately leads to centralization of fetal blood circulation [3], which is aggravated during labor, leads to hypoperfusion of organs and tissues, especially those not included in vital. One of these tissues is muscular tissue, which constitutes 23-25% of the whole body weight in full-term newborns [24].
We consider one of the reasons for the development of asphyxia in newborns (96.6% of children) to congenital damage to the muscles involved in the act of breathing (diaphragm, intercostal, spinal), which differentiate during ontogenesis among the first [24]. The development of the degenerative-dystrophic process in these muscles by the time of birth is quite pronounced. This prevents the timely inclusion of the respiratory muscles in the work during the first breath and hinders its optimal functioning in the postnatal period.
The formation of muscle contractures is the inevitable outcome of congenital « myofibrillosis » [12], the difference in different children consists only in the severity of the process and the rate of its progression. « With an unfavorable course of the disease by 5-6 months -1 year, with a favorable one – by 3-5 years … … most children with cerebral palsy develop persistent contractures and deformities in the joints of the limbs » [17].
Children with severe forms of the disease constitute a risk group for the early formation of muscle contractures and need the advice of specialists from the Institute of Clinical Rehabilitation, with a view to deciding on the surgical treatment using a step-by-step fibrotomy.
FINDINGS:
In children of the studied group admitted to the 1st stage of treatment at the institute, there is an intrauterine onset of the pathological condition expressed in the appearance of movement disorders, regarded as a manifestation of cerebral palsy.
With the advent of hidden and overt contractures, the effect of complex conservative therapy is, at best, temporary, often absent. Its low effectiveness is due to the presence of a diffuse cicatricial process in the muscles, and cicatricial tissue becomes less stretchable with age, and motor impairment progresses.
The very concept of the effectiveness of conservative therapy involves an element of conditionality and relativity, since the development of motor skills in every patient with cerebral palsy is ultimately determined by a certain “threshold” of opportunities, which depends only on the ability of the preserved structures to compensate for the functions of the dead and damaged. Successful conservative treatment affects the pace of approaching this « threshold », allows you to stay within the achieved level of motor development, which can be exceeded only by eliminating contractures and deformities of the joints by surgery.
Already at an early stage in the development of contractures, these children need their adequate orthopedic correction followed by therapeutic gymnastics, massage, hydraulic procedures, etc. Method of phased fibrotomy in Ulzibat VB allows this to be done [20].
“Large” orthopedic operations are relatively or absolutely contraindicated to more than half of the children who applied to the Institute of Clinical Rehabilitation for a number of indicators: multiplicity and severe degree of contracture of the joints, lesion in the form of tetraparesis, hyperkinetic form, lack of persistent, well-marked adjusting straightening reflexes, the presence of deep intellectual delay and speech development, etc. [16]. That is why the method of phased fibrotomy is the method of choice for this category of patients, used in outpatient conditions.
Intervention at the stage of appearance of muscle contractures is optimal, as persistent contractures and deformities of the joints require more traumatic operations and inpatient treatment.
Evaluation of the emotional profile of a sick child has important diagnostic and prognostic value when using a surgical method of treatment.
« Therapy started as early as possible gives the maximum effect » [17]. This fully applies to the stepwise fibrotomy method.
We do not claim the exceptional role of the method of phased fibrotomy in the treatment of patients with cerebral palsy, but we believe that its place in the general system of rehabilitation measures should be determined.
So what is the difference between :
Percs?? (dr Matthew Dobbs)
for muscle/tendon lengthening to relieve contracture (limited motion) in joints.
I honestly can’t find good full scientific description yes I wish to read ….in order to understand this operation …. don’t understand haw to compare without theory and scientific explanation…..
I read all I have found so I can’t figure out diference between ??????
Splm = dr Nuzzo opération ( not enough scientific publications as well for me ) Haw ulzibat method is different from SPLM dr Nuzzo method from USA ? Not sure haw to answer…..
Here study of SPLM dr Nuzzo operation ( yes clinical study exist):
http://e-n-a.gr/uploads/1-s2.0-S0891842209001323.pdf
(( I am Russian so I can see ulzibat publications in Russian about his method)
Here you can see about Splm :
( so explain me the diference?)
http://www.pediatric-orthopedics.com/Treatments/Muscle_Surgery/Perc_Lengthening/perc_lengthening.html
I know this Ulzibat methode and Dr. Nuzzo Splm looks for me very much the same!
I am just a mother 😉
But I see that both methods are very similar and was started in 1987 ulzibat ( had his patent in URSS yet) as Nuzzo started in the 70‘ies. I think he did it first and Ulzibat modified the technique….( only my reflection)
And
Ulzibat ( publications only in Russian it’s ok for me but as I promised hire I translated just a small part ….
If you want to know about Ulzibat watch this as well :
(A lot of tv news in Russia and a lot of testimonials from parents)
On russian tv in news ( Ulzibat methode 60 opérations in 3 days in habarovsk) yes come from Tula to habarovsk and team did 60 operations in 3 days for children’s with Cp….
So honestly I think it’s very serious method in Russia ( all in order legally) with patents for method and equipment :
Hire dr Ulzibat dissertation published for his method :
http://medical-diss.com/docreader/454260/a?#?page=3
Hire one of patents :
So no it’s obviously not taken off «completely » spasticity …no it’s orthopedic operation it’s relive scar tissue at the site of necrosis only ( it’s not cutting mussels it’s only very small scar tissue)
This video explain : https://youtu.be/n4d_WFw0GdA
And if we talking about laws and legality to do this method:
During 1998 in the leading clinics of the country:
– Department of Traumatology and Orthopedics, Faculty of Postgraduate Education, Moscow Medical Academy. THEM. Sechenov;
– Department of Pediatric Surgery, Russian State Medical University;
– Department of Cerebral Palsy of the Russian Research Children’s Orthopedic Institute named after G.I. Turner
a clinical demonstration of the method and medical tests of a special surgical instrument – Microfibrillot, which is used to carry out a complex of low-impact operations. ”
And further: “After the demonstration of the method to a representative of the Russian Research Children’s Orthopedic Institute. GI, Turner, Head of the Department of Surgery for Cerebral Palsy, Ph.D. A.P. Kutuzov in Tula held a demonstration of the method at the very base of this institute.
In conclusion, the director of the institute, MD. prof. Yu.I. Pozdnikina noted that the use of new surgical technology should be made as early as possible, the interventions performed are adequate, effective, can be performed on an outpatient basis by trained specialists.
In a letter to the Deputy Minister of Health of the Russian Federation V.I. Starodubova Professor Yu.I. Pozdnikin proposed the creation of an extrabudgetary research team with our non-state health care facilities to conduct joint research and develop a number of provisions that can be used both in the practice of the institute and for the introduction of methods into Russian medical institutions, thereby taking part in the development and improvement of outpatient orthopedic care. children in order to implement the provisions of the “Concept of development of health care and medical science in the Russian Federation”.
Dissertation of dr Nasarov ( one of doctors which was teached by Ulzibat)
http://miotenofasciotomia.com/wp-content/uploads/2018/07/tesis-rus.pdf
in fact Ulzibat wasn’t the only surgeon to operate with his method he teached 5 others Russian doctors and they are not all waiting in Tula when all Russian cp children’s comes to them , they are doing external operations -so going in local hospital in diferent cuties in regions of Russia and yes doing 60-100 operations in 3-4 days ….
But honestly for CP problem is not in mussels
Or even not in spinal connections ( but yes if child suffer from pain what we have to do ?
To relise his pain….. and obviously – choise of what is the best to do is on parents and it’s will depends of level of haw child is affected by CP …and in what way….)
Cp Problem is in Brain !!!! But we all know it ….
So all I know which can helps Brain it’s 3 things:
1) It’s hbot (Hyperbare) and we have a lot really a lot scientific publications haw it can help :
Just try to watch this Israel’s Professor presentation :
Video is in English do listen it:
( need read more about Hyperbare ask me I give you more on my blog to read)
2) it’s PoNS Device (PoNS is a device for translingual electrical stimulation of the brain that enhances the brain’s natural ability to repair damaged areas and form new functional pathways.)
Need more – again ask me 😉
And
3) it’s stem cells
But it’s in clinical trails in Duke University but progress is real you can see it on Duke parents fb page…. and yes we also gave scientific publications from Joanne Kurtzberg, MD
Director, Carolinas Cord Blood Bank
Chief Scientific Officer, Robertson Clinical and Translational Cell Therapy Program
Director, Pediatric Blood and Marrow Transplant Program
